Anatomy & Function
Every person has two cruciate ligaments in each knee joint - an anterior and a posterior cruciate ligament. The name is derived from the structure of the ligaments, which run into each other in a cross shape and are about three to five centimetres long. The cruciate ligament is one of the most important structures in the knee joint and is necessary for the stability of the knee joint as well as for harmonious movement. The anterior cruciate ligament tears in over 90% of cases.
A tear of the anterior cruciateligament (ACL) often occurs in the context of a "non-contact injury" (without external impact) - for example, when the knee joint is hyperextended or twisted while the thigh muscles are tense. Anterior cruciate ligament rupture often occurs in sports with rapid changes of direction, such as football or other ball sports, as well as in skiing, when the leg twists when the muscles and ligaments are tense.
Symptoms & Complaints
The knee with its cartilaginous surfaces and ligaments is a complicated joint and very susceptible to injury, especially in certain sports. It is not uncommon for one of the two cruciate ligaments to be affected, usually the anterior one.
Signs of an anterior cruciate ligament tear can be:
- Tearing sensation with "plop sound".
- Effusion formation in the knee joint immediately, also possible with a delay
- Knee pain
- Inhibition of stretching and bending - Impairment of mobility
- Reduction of the load capacity
- Gait insecurity - feeling of instability
Causes
One out of every 1000 people between the ages of 15 and 25 ruptures a cruciate ligament every year.
Major risk factors are:
- landing on one leg after a jump (e.g. landing after a header or throw)
- fixed foot and body weight distribution over the injured leg (e.g. dribbling)
- sudden stopping with simultaneous turning movement, simultaneous change of direction (e.g. when trying to defend oneself)
- sudden stop and simultaneous long lunge (e.g. forced change of direction after feinting the opponent)
- Lateral readjustment steps during braking (e.g. as part of a defence attempt).
- the hyperextension in the knee joint, e .g. landing after jumping) (valgus landing)
Diagnosis
The diagnosis of ACL rupture in freshly injured patients is a challenge for examiners. Since the functional status in particular must be assessed, the clinical examination has priority. Although an MRI scan indicates an ACL injury, differentiation between partial and complete rupture is often difficult.
Biomechanics of the intact anterior cruciate ligament
The main function of the ACL is both to stabilise against a forward force of the lower leg (anterior tibial translation (ATT) force) and to maintain rotational stability of the knee joint. These two stabilisation tasks can be investigated using the Lachman test and the pivot shift test.
Lachman test
Pivot Shift Test
Graduation of the Pivot Shift Test
In addition to the Lachman test, the pivot shift test is a standardised procedure when a torn anterior cruciate ligament is suspected. The test has the advantage that it can also contribute in particular to the assessment of the anterolateral knee joint stability, the anterolateral ligament complex, and thus to further differentiated surgical planning.
We perform the test in 3 different leg positions:
- Grade 1: Pivot shift positive in internal rotation of the lower leg
- Grade 2: Pivot Shift positive in internal rotation and neutral position of the lower leg.
- Grade 3: Pivot shift positive in external rotation and neutral position of the lower leg, less in internal rotation.
The basic principle of the test is the internal rotation of the lower leg and thus of the tibial plateau against the thigh. Normally, the cruciate ligaments wrap around each other in such a way that further internal rotation and forward displacement of the tibia is prevented. If, on the other hand, there is a lesion of the anterior cruciate ligament, internal rotation causes the tibial head to shift forward and the centre of rotation of the knee joint to shift inwards (see axis of rotation).
Test performance (patient lying on his/her back):
- The examiner grasps the back of the foot or the sole of the foot of the person being examined with one hand.
- With the other hand, grasp the lower leg from below (the thumb comes to rest on the head of the fibula).
- the examiner now lifts the stretched leg of the person to be treated up to a hip flexion of 20
- with the "heel hand" the lower leg is now turned inwards and axial pressure is exerted towards the hip
- With the hand on the head of the fibula, an "X leg stress" is exerted on the knee joint.
- the examiner now slowly bends the leg at the knee joint
The test is positive (positive pivot shift test) if there is a jerking back of the tibial plateau, which was previously shifted forward, during flexion of 20- 40 degrees. This "snap" in the knee is less unpleasant for the patient in the chronic stage.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI) produces cross-sectional images of the body. This method is based on the application of a strong magnetic field and radio waves. There is no radiation exposure for patients. During an MRI examination, the cruciate ligaments in particular can be depicted very precisely. For this reason, an MRI is very suitable for detecting a cruciate ligament tear. In some cases, however, a cruciate ligament tear is present even though it is not visible on the MRI images and vice versa. In these cases, the MRI should be considered false. The number of false MRI's depends on the quality of the MRI images and the diagnostician (radiologist / orthopedist).
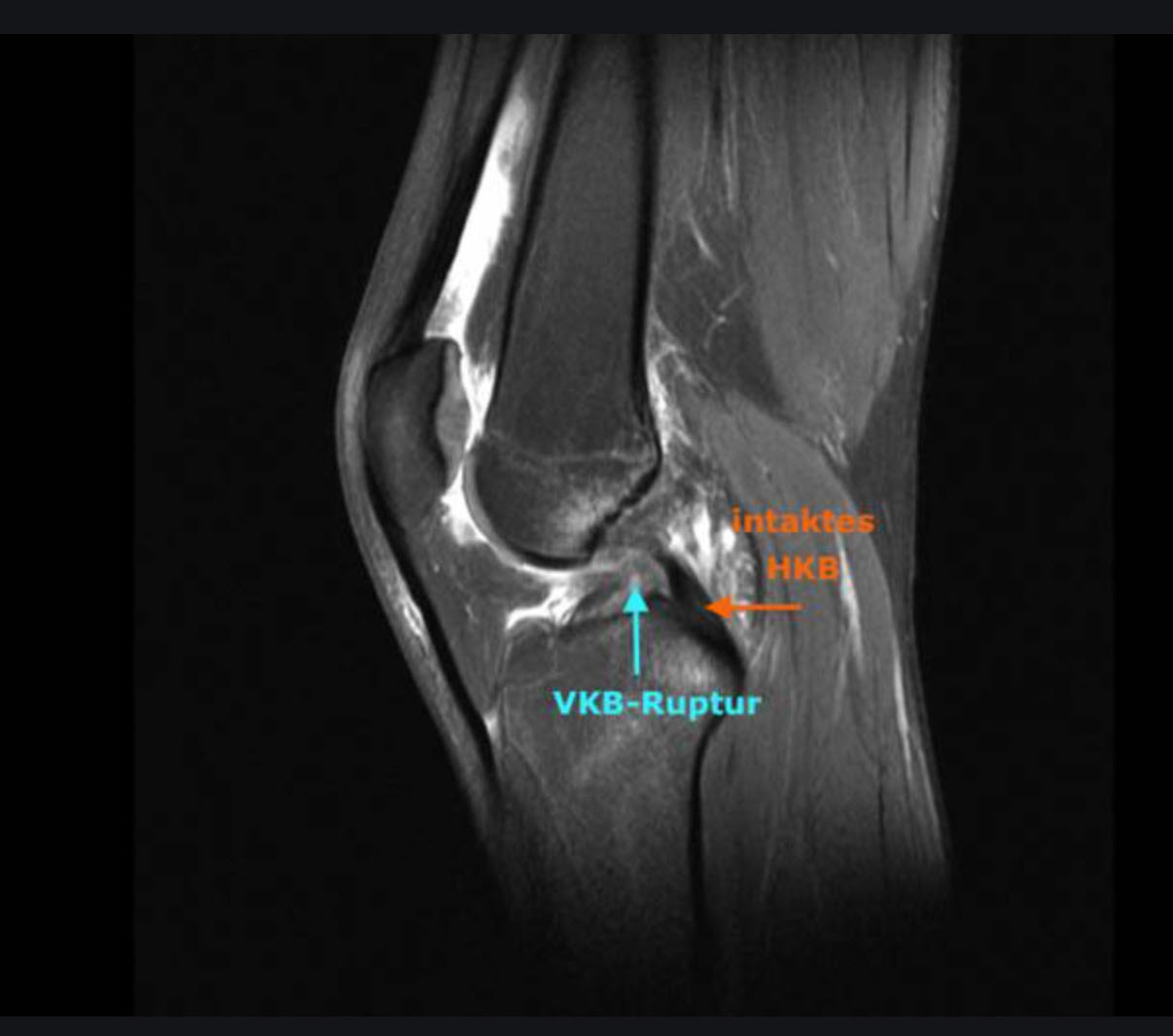
MRI image of a rupture of the anterior cruciate ligament
Treatment
Cruciate ligament ruptures can be treated both conservatively and surgically. The indication for a ligamentoplasty depends on various factors, e.g. how severe the pain and suffering of the affected person is, the mobility of the joint is impaired, there is uncertainty when walking and also the sporting ambition is a decisive factor for us.
Conservative therapy
Basically, conservative treatment aims to eliminate the pain, restore mobility, resilience and stability of the knee joint.
The following therapies are possible:
- Drug treatment: Drug treatment aims to relieve the pain or make it disappear completely.
- Physiotherapy: Physiotherapy- Special exercises to strengthen the muscles, mobilisation and exercises to improve landing techniques.
- Physical measures: e.g. electrotherapy , cold treatment
- Aids: e.g. walkingaids, knee supports, orthoses
Operation
If there is no improvement of the pain within the framework of conservative treatment and if the restriction of movement and load with signs of instability (Giving Way signs) persists, surgical stabilisation is recommended. All surgical procedures can usually be performed arthroscopically, minimally invasively, by means of arthroscopy.
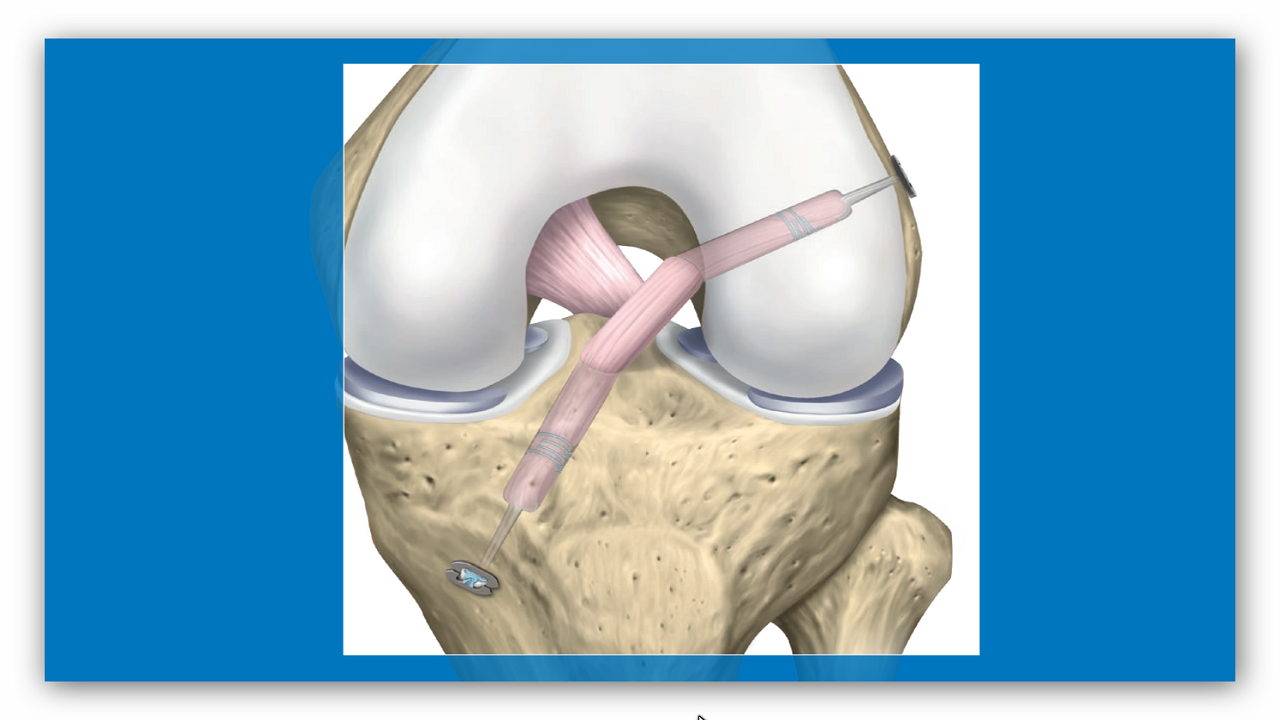
Arthroscopically assisted cruciate ligament reconstruction
At the beginning of arthroscopically assisted cruciate ligament reconstruction, an arthroscopy of the knee joint (syn. arthroscopy), a minimally invasive diagnostic and/or therapeutic treatment of joints via small incisions (arthrotomies) using an endoscope, is first performed. This procedure gives us an indication of other possible damage in the knee joint, such as meniscus lesions or cartilage defects, and describes the type and localisation of the tear in the cruciate ligament. We distinguish between several surgical procedures (minimally invasive) for the treatment of cruciate ligament rupture:
Preservation of the own cruciate ligament: "Internal Bracing
In certain fresh tears of the anterior cruciate ligament near the thigh - type I and II of the Sherman classification - we are increasingly using the internal bracing procedure. This offers patients the chance to preserve the torn cruciate ligament. Internal bracing is an internal splinting procedure that allows the torn cruciate ligament to follow its original path. The torn cruciate ligament on the thigh is first grasped with sutures and reattached to the thigh using a special transosseous technique. For this purpose, we use the self-healing potential after an acute cruciate ligament tear and thus enable structured and targeted healing between the cruciate ligament stumps. Subsequently, a stable "internal splinting" is carried out with the Internal Brace technique, so that not only the own cruciate ligament with all important nerve endings is preserved, but also a very early load-bearing capacity of the knee joint is made possible with a significantly shortened rehabilitation time.
Augmentation of the partial rupture of the anterior cruciate ligament
The anterior cruciate ligament (ACL) consists of several parallel fibres, which are divided into anteromedial (AM: more anterior and towards the centre) and posterolateral (PL: posterior,lateral) fibres. The AM fibres or AM bundles stabilise the knee joint mainly in flexion, especially against excessive forward displacement of the tibia, while the PL fibres or PL bundles stabilise near extension and protect stability during rotational movements of the knee joint. According to Jack Hughston's principle: "Repair what is torn", we replace one of the torn AM or PL bundles in the case of partial ruptures of the anterior cruciate ligament and leave the intact, functional bundle untouched. Depending on the condition of the remaining tissue of the ligament, we support the biological healing process with an internal bracing.
Reconstruction of the anterior cruciate ligament rupture
In the case of a complete tear of the anterior cruciate ligament, the semitendinosus/gracilis tendon (STG) or even the isolated semitendinosus tendon as a triple or quadruple sling as a ligament replacement is currently the method of choice.
Everything at a glance:
- Operation time: 45-60 min.
- Anaesthesia: General or Spinal
- Hospital stay: outpatient and inpatient
- Fit for work: after 2-10 weeks
- return to sports (RTS): 6-10 months
Our recommendations for anterior cruciate ligament reconstruction:
- in athletes who play high-impact sports, such as soccer, rugby, handball, volleyball, basketball, tennis, dancing, skiing and also intensive aerobics.
- In the case of subjectively complained instability with the so-called giving-way phenomenon, even after conservative treatment.
- In the case of repeated effusions and swellings, which undoubtedly show instability as the primary cause of the complaints.
- For concomitant injuries such as tearing of the meniscus, cartilage damage, etc.
- In the case of concomitant injuries of the periphery such as capsule-ligament injuries (e.g. anterolateral ligament, higher-grade medial-external ligament injuries, etc.).
- In the case of intrinsic (congenital) factors such as hypermobility, hyperextensibility of the knee joint, pronounced weakness of the connective tissue, etc.
- if patients wish to be able to perform sports and occupational activities that put a strain on their knees
Our preferred surgical procedure
In addition to advances in surgical technique, the following points are also decisive for the success of the operation:
- The drill channel positioning of both the femur and the tibia has been optimised. Today, in order to achieve an anatomical fixation of the ACL, the drill channel of the lower leg bone is positioned independently of that of the upper leg.
- The drill hole of the lower leg is in the centre of the attachment area of the anterior cruciate ligament.
- The placement of the drill channels is based on anatomical landmarks.
Taking into account these and other relevant principles such as choice of graft, timing of surgery, fixation technique and post-treatment, very good results (over 95% success rate) can be achieved at the present time with this surgical procedure favoured by us.
Aftercare
At the centre of post-cruciate ligament reconstruction treatment are various treatment phases that characterise different focal points, such as the acute wound healing phase, the time of tendon healing in the bone canals, the transformation time of the tendon into a ligament structure and the phase of eliminating muscular and neuromuscular deficits. The aim of these treatments is active knee stabilisation, the achievement of full mobility and axis-appropriate loading, in order to then prepare for sport-specific training by creating the conditional and coordinative foundations. Only after full muscular and neuromuscular control has been achieved and the reconstruction processes of the tendon graft have been completed is a low-risk return to weight-bearing sports advisable.
Treatment calendar anterior cruciate ligament reconstruction
Your treatment roadmap after cruciate ligament reconstruction. An individualised aftercare concept for arthroscopic surgery of anterior cruciate ligament reconstruction.
→ Treatment calendar anterior cruciate ligament reconstruction
Treatment calendar Anterior cruciate ligament reconstruction with meniscus suture
Your treatment plan after cruciate ligament reconstruction with meniscus suture. An individualised aftercare concept for arthroscopic cruciate ligament reconstruction with meniscus suture.
→ Treatment calendar Anterior cruciate ligament reconstruction with meniscus suture
FAQs
Due to increasing sporting activity, the number of cruciate ligament injuries in Germany is constantly rising. In our consultation hours, we find that many patients have similar questions. Therefore, we have compiled the most common points that come up during a detailed consultation for your information.