Anatomy & Function
Anterolateral ligament complex (ALL) - today's almost exclusively arthroscopic treatment of cruciate ligament injuries has more or less replaced open knee ligament surgery. At the same time, we as physicians are repeatedly confronted with combined and complex instabilities of the knee joint in which isolated reconstruction of the cruciate ligaments is not sufficient. Thus, an underestimated peripheral instability ( internal-external ligament-anterolateral ligament, etc.) can affect the result of a possibly good anterior cruciate ligament reconstruction.
Symptoms & Complaints
Failure rate of anterior cruciate ligament surgery is high - the majority of football players with anterior cruciate ligament(ACL) injury opt for surgery with reconstruction of the anterior cruciate ligament (ACL surgery). Many achieve their original level of performance and can return to play without difficulty. However, approximately 20-25% of male and female athletes with surgically repaired ACL suffer a re-injury with a new tear of the ACL or the ACL loses its strength and stability (anterior cruciate ligament insufficiency). The results of these failures are multifactorial, but a major one is the so-called.anterolateral rotational instability, which may not have been restored or recognized during cruciate ligament reconstruction.
Knee surgeons describe new ligament at the knee joint, the "anterolateral ligament" - the safety belt for the anterior cruciate ligament?
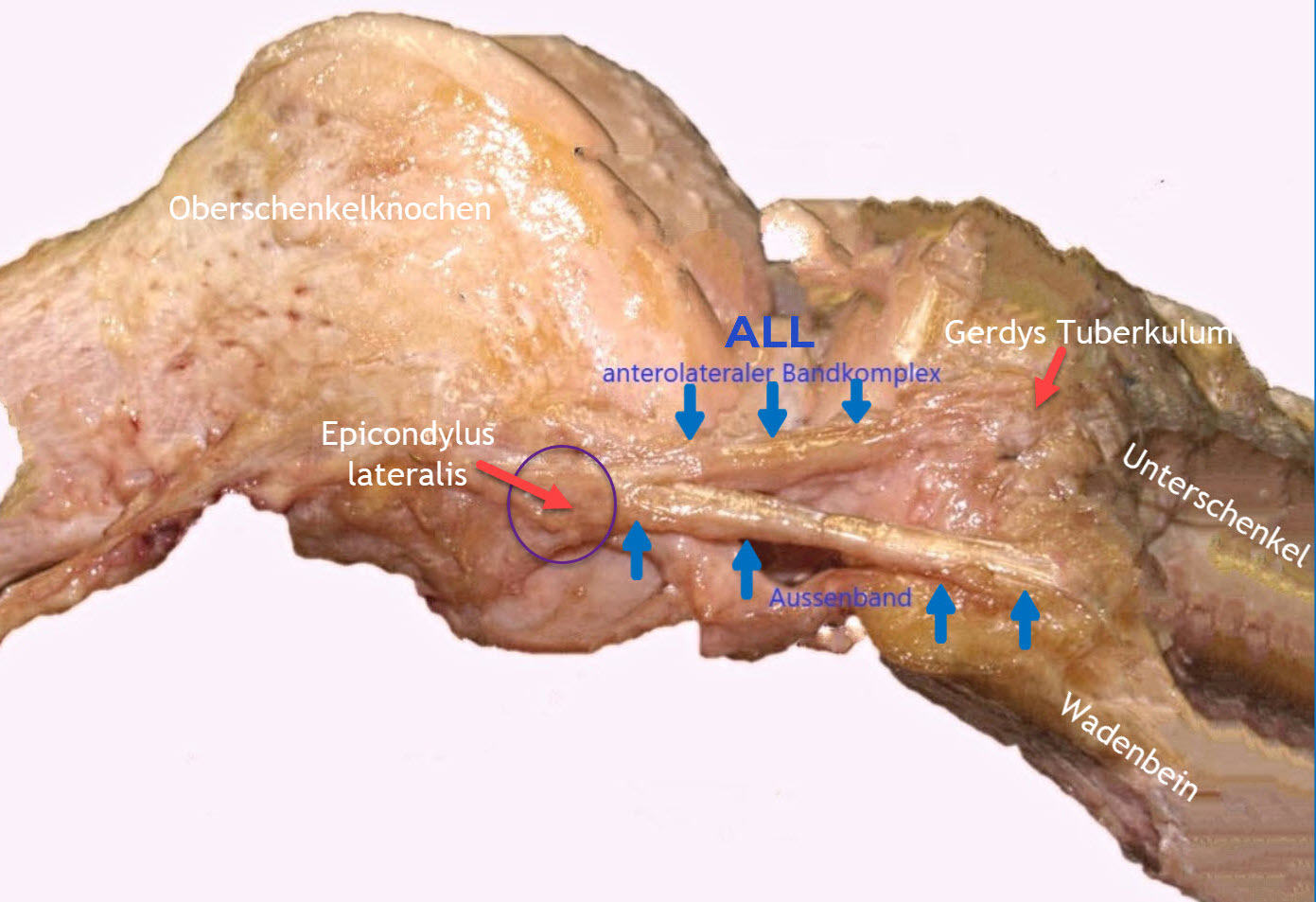
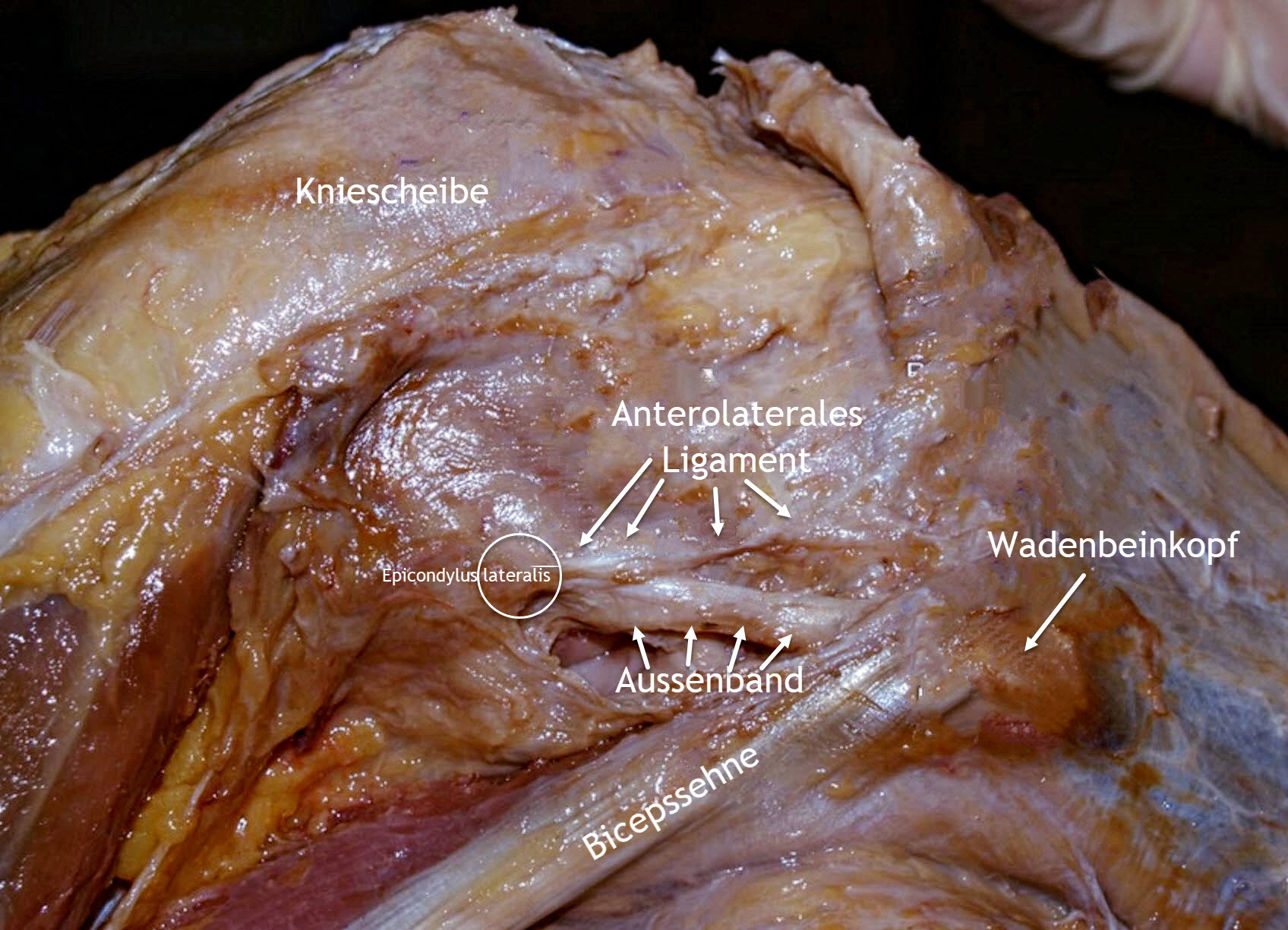
For example, in 2013, Dr. Steven Claes , one of the two knee surgeons, described a fibrous ligament as part of his studies that can be injured when the anterior cruciate ligament is torn. Anatomically, the ligament or ligament complex runs on the outside of the knee joint and presumably several anatomical structures can be held responsible, including the iliotibial band complex , the anterolateral ligament and the Kaplan fibers. The essential function of the ligament is to maintain rotational stability, especially during internal rotation of the knee joint. Reconstruction of this ligament can successfully improve overall stability in patients with high-grade pivot shift phenomenon or in patients with persistent pivot shift after cruciate ligament reconstruction. The ligament often eludes visualization in magnetic resonance imaging findings, so that if there is a suspicion of this in the clinical examination (stability testing), the indication for ACL reconstruction is made by the surgeon after compliance with specific criteria.
Causes
What happens in the knee joint after ACL rupture? Motion kinematic studies show the changes in the knee joint after complete rupture of the anterior cruciate ligament:
After complete severing or tearing of the anterior cruciate ligament, an anterior knee joint instability occurs with increased forward force of the lower leg (anterior tibial translation). As a result of the existing anterior instability of the knee joint, there is a forward displacement (subluxation) of the lower leg (tibia) when the knee joint is loaded. In addition to anterior instability, an ACL rupture also causes what is known as anterolateral rotational instability. This instability is characterized by a shift of the center of rotation to the inner joint section. This increases the mobility of the outer lower leg (lateral tibial plateau) due to an increased forward force and extended internal rotation.
Displacement of the rotation axis after ACL rupture
Centre of rotation of the knee joint with intact anterior cruciate ligament:
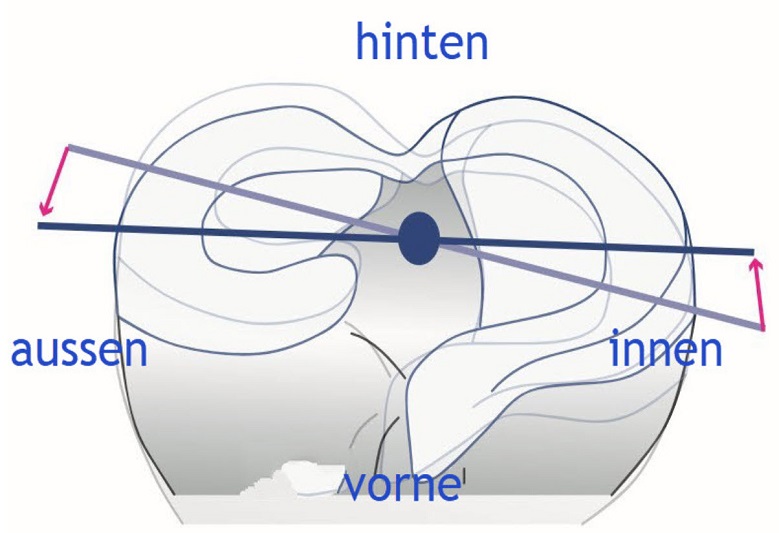
central axis of rotation
Centre of rotation of the knee joint in anterior cruciate ligament rupture:
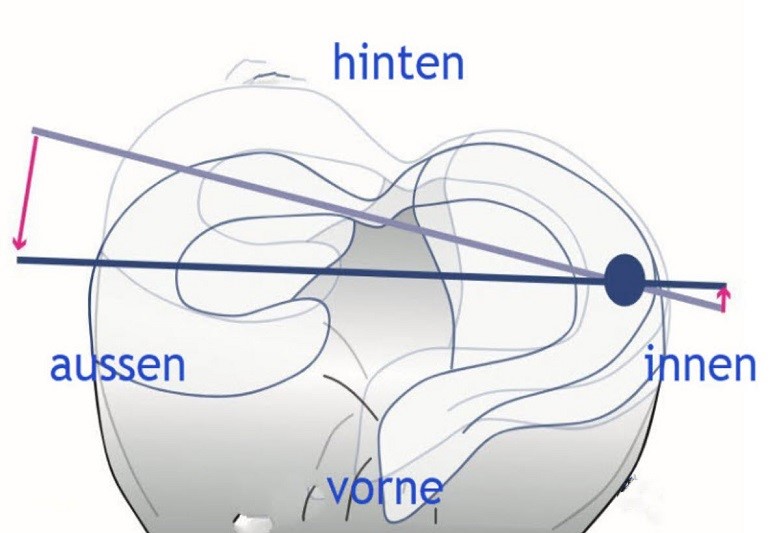
Shift inwards
Alteration of the rotation axis in anterior cruciate ligament rupture:
Click on the button to load the content from imgflip.com.
Central inwards
Biomechanics of the intact anterior cruciate ligament
The main task of the ACL is both to stabilise against a forward force of the lower leg (anterior tibial translation (ATT) force) and to maintain rotational stability of the knee joint. These two stabilisation tasks can be investigated using the Lachman and pivot shift tests:
Diagnosis
The diagnosis of anterolateral ligamentous complex (ALL) injury can be challenging even for specialists. Historically, the first observations of the anterolateral ligament complex (ALL) can be attributed to French anatomist Paul Segond . In 1897, he reported a "nacreous fiber resistant ligament" that showed extreme stress under excessive internal rotation of the lower leg, which eventually led to an avulsion fracture (an avulsion fracture is a bone fracture , in which a bone fragment is torn from the bone by the strong pull on a tendon anchored in the bone) as a result of a strong rotational stress. Later examinations showed that this avulsion fracture ("Segond fracture") was an indirect sign of an anterior cruciate ligament tear.
An appropriate diagnosis can only be obtained with a detailed history describing the mechanism of trauma, a careful clinical examination, and appropriate evaluation of radiographic and MRI imaging.
In general, the combined injury of the anterior cruciate ligament and anterolateral ligament complex (ALL) is similar to that of an isolated anterior cruciate ligament rupture (ACL rupture). Contact and non-contact mostly athletic injuries with early flexion, increased X-leg loading (dynamic valgus) and internal rotation of the lower leg (internal rotation), are frequently reported. Was e.g. landing after a header in almost full extension of the knee joint, bending of the knee joint to the inside during equilibrium shift - disturbance or perhaps stopping after change of direction responsible for the accident event? These questions are eminently important, since meticulous reconstruction of the accident mechanism usually points to the injured structure of the knee joint. It is helpful if relatives or friends have been able to make video recordings of the accident using a smartphone or camera.
During the examination, the lateral compartment of the knee should be carefully examined. Any swelling with tenderness over the lateral aspect of the knee, especially if proximal to the head of the fibula but also below the external joint space, should be assessed. In addition, the integrity of all ligaments and menisci (medial collateral ligament-posterior cruciate ligament, medial external meniscus, etc) should be assessed.
If patient compliance allows safe and effective assessment of ACL and ALL integrity, above laxity tests can be performed already in the acute phase. However, assessment is more effective in the later subacute and chronic phases after swelling and pain have subsided.
Graduation of the Pivot Shift Test
The pivot shift test is a standardised procedure when a torn anterior cruciate ligament is suspected. The test has the advantage that it can also contribute in particular to the assessment of the anterolateral knee joint stability, the anterolateral ligament complex, and thus to further differentiated surgical planning.
We perform the test in 3 different leg positions:
- Pivot shift positive in internal rotation of the lower leg (grade 1)
- Pivot shift positive in internal rotation and neutral position of the lower leg (grade 2)
- Pivot shift positive in external rotation and neutral position of the lower leg, less in internal rotation (grade 3).
A pivot shift test in grade 2 and 3 is a decisive (primary) criterion for testing and possible implementation of stabilisation of the anterolateral ligament complex (ALL).
The basic principle of the test is the internal rotation of the lower leg and thus of the tibial plateau against the thigh. Normally, the cruciate ligaments wrap around each other in such a way that further internal rotation and forward displacement of the tibia is prevented. If, on the other hand, there is a lesion of the anterior cruciate ligament, internal rotation causes the tibial head to shift forward and the centre of rotation of the knee joint to shift inwards (see axis of rotation).
Test performance (patient lying on his/her back):
- The examiner grasps the back of the foot or the sole of the foot of the person being examined with one hand.
- With the other hand, grasp the lower leg from below (the thumb comes to rest on the head of the fibula).
- The examiner now lifts the patient's extended leg to a hip flexion of 20°.
- with the "heel hand" the lower leg is now turned inwards and axial pressure is exerted towards the hip
- with the hand on the head of the fibula, an "X leg stress" is exerted on the knee joint
- the examiner now slowly bends the leg at the knee joint
The test is positive (positive pivot shift test) if:
- at a flexion of 20- 40 degrees, there is a jerking back of the tibial plateau, which was previously shifted forward. This "snap" in the knee is less unpleasant for patients in the chronic stage.
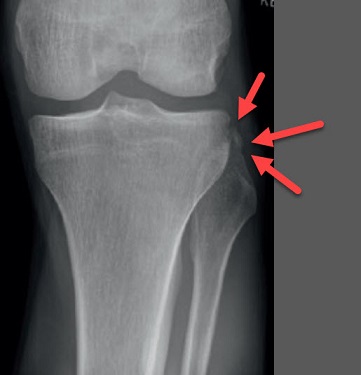
X-ray
The clinical diagnosis of an ALL injury can be supported by an X-ray. As described above, a "Segond fracture" represents a bony injury to the ALL attachment to the tibial head. A "Segond fracture" refers to the avulsion of a bony fragment of the tibial head, slightly offset from Gerdys tubercle. A "Segond fracture" can be caused by high traction forces of the ALL and is often the result of internal rotation of the knee and possibly "X-leg loading" (varus loading). Such fractures can be visualised on straight radiographs of the knee.
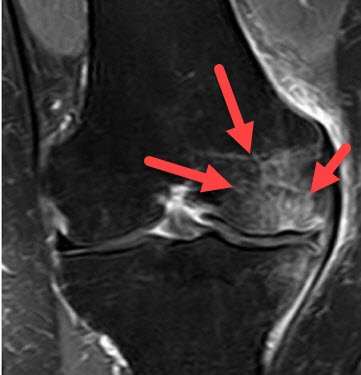
Magnetic resonance tomogram
Two studies have shown that ALL abnormalities are often found in the tibial part of the ligament on MRI scans, although there is still some controversy. For example, a lesion of the anterolateral stabilising structures is currently not directly detectable on MRI.
But indirect signs on the MRI may indicate an injury to the ALL:
- The presence of marrow edema secondary to recent and severe pivot-shift trauma; in the acute posttraumatic phase, marrow edema is seen in the outer femur and often on both sides on the posterior tibial plateau.
Sonography
Sonography may be of additional value in diagnosing ALL injury. Again, the portion of the ligament near the lower leg is better visualized than the femoral portion, and the portion that attaches to the lateral meniscus is difficult to identify. Because most ALL tears occur in the portion near the tibia, ultrasound can be a useful diagnostic tool for visualizing ALL injuries

Treatment
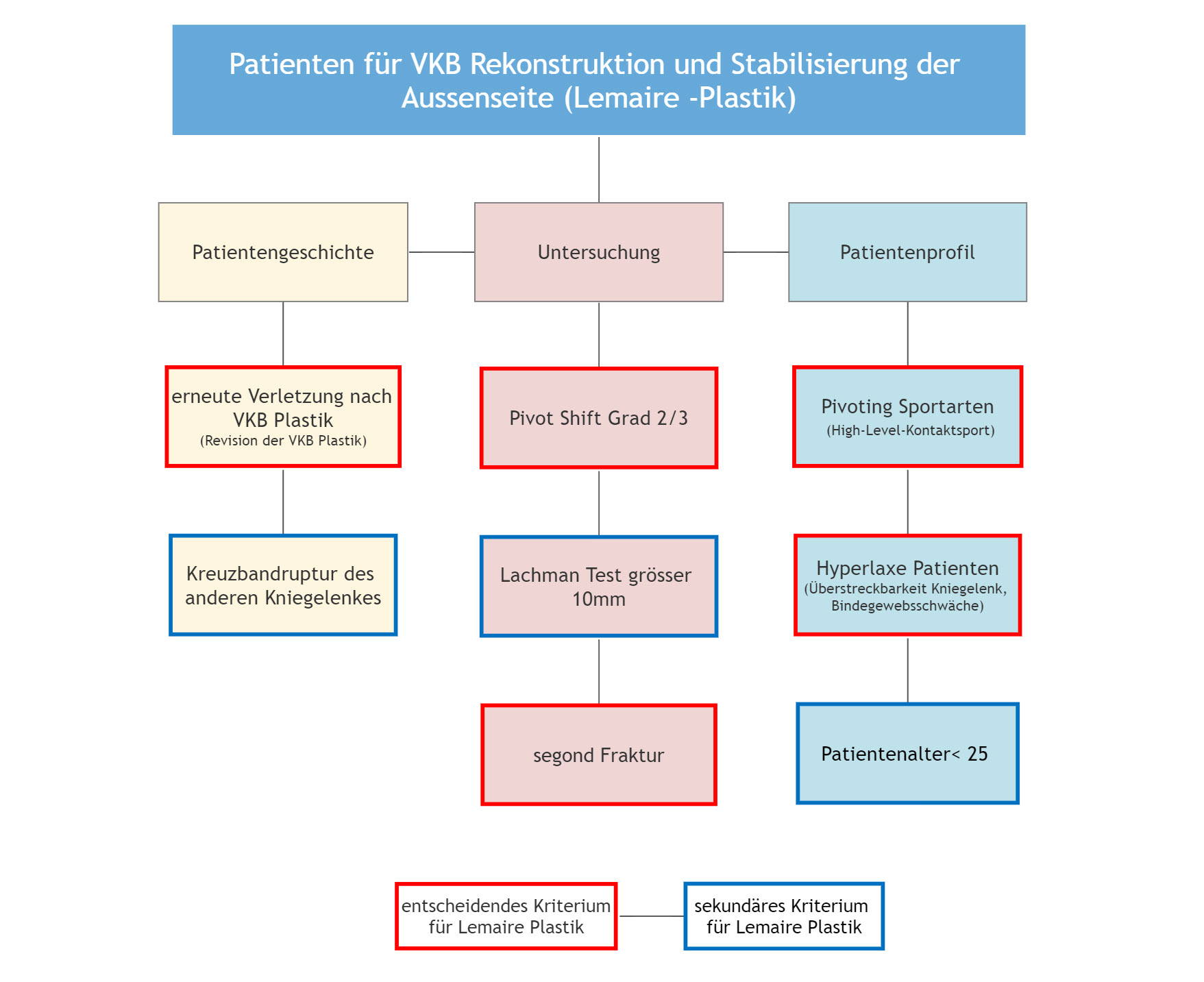
Guidelines for the treatment of anterolateral instability. They are based on the consensus paper of the Ligament Expert Group (consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee). Requirements for anterolateral ligament complex (ALL) surgery in anterior cruciate ligament (ACL) reconstruction. According to the ALL expert group, at least one primary or two secondary criteria should be present.
Decisive primary criterion:
- Re-injury after ACL plastic
- pivot Shift Grade 2 and 3
- high level contact sports
- hyperlaxe, patients with weak connective tissue
- segond fracture
Secondary criterion:
- Cruciate ligament rupture of the other knee joint
- Lachman test greater than 10 mm (side comparison)
- Patient age less than 25 years
Operation anterolateral ligament complex (ALL)
The treatment of anterior cruciate ligament (ACL) rupture alone is not sufficient in some cases and a remaining anterolateral (rotational) instability (up to 20-25%) leads to less good functional results in the affected patients. Combined injuries of the ACL and the anterolateral complex (ALL) should thus be treated in a joint procedure to avoid the aforementioned rotational instability.
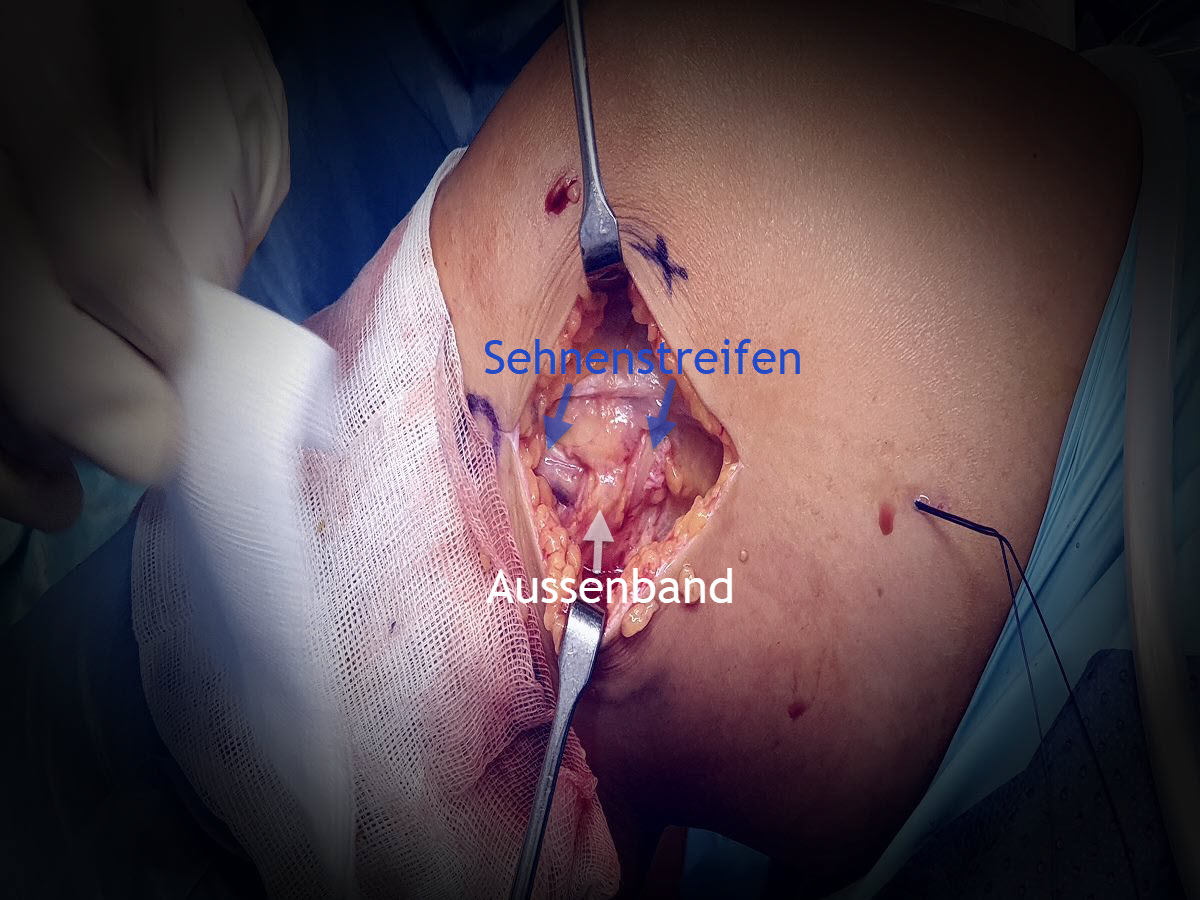
The surgical principle is to improve the rotational instability of an unstable knee joint damaged by anterior cruciate ligament rupture. The technique described here is the modified Lemaire procedure (so-called lateral tenodesis) with a less invasive approach, in which a small strip of tendon of the iliotibial band (ITB) is fixed at the isometric point on the epicondylus lateralis by a dissolvable screw.
Our surgical procedure for anterolateral rotational instability
Aftercare
More information will follow shortly.